Doctors failed to tell a father of seven that he had a terminal illness and gave him false reassurance that he would be all right, an investigation by England’s Health Ombudsman has found.
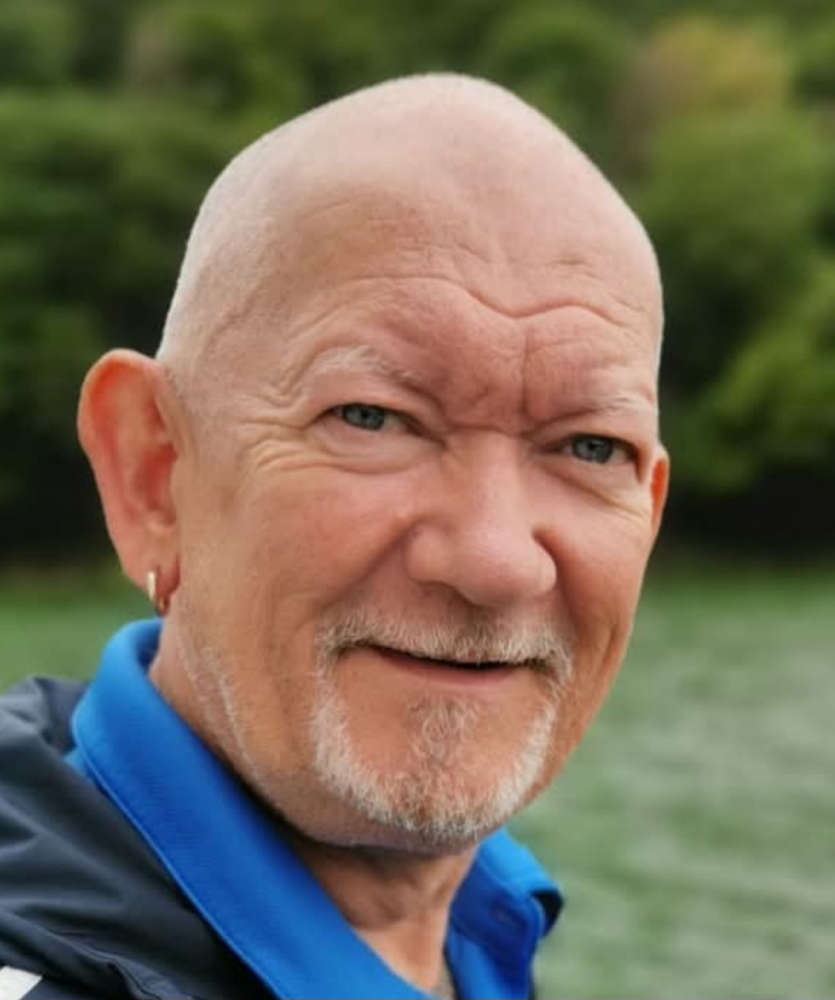
William Chapman, known as Syd, died eight months after accidentally discovering his prognosis when his GP, believing hospital doctors had already told him the full scale of his condition, mentioned it during a phone call.
The Parliamentary and Health Service Ombudsman (PHSO) said that the doctors at the Countess of Chester Hospital showed a worrying lack of accountability and had failed to learn from the mistakes made in Syd’s case.
Our investigation highlights how quickly trust can be eroded in public services and why NHS and Government leaders need to make sure they build and support a consistent culture of openness and honesty within the NHS.
Rebecca Hilsenrath KC (Hon), Chief Executive Officer at PHSO, said:
“There are many brilliant and dedicated people working in the challenging circumstances of an NHS under intense pressure. But it is inevitable that sometimes things go wrong. When that happens, it is important that people listen and take learning on board.
“This disturbing case highlights the importance of effective communication and the consequences of getting it wrong. When you hear this kind of diagnosis in this kind in this way, you lose a sense of dignity and the opportunity to make your own decisions about how to live your life. The family’s trauma was compounded by their treatment during the hospital’s internal complaints handling.
“Too little accountability and too much defensiveness in the NHS is something we highlighted in our Broken Trust report two years ago. There needs to be a cultural shift starting from the top down to improve patient safety and avoid further harm to patients and their families.
“Good communication is critical in health settings. In this case, a patient was misinformed about his health and this led to a breakdown in trust between clinicians and the patient and to prolonged distress for his family.”
Syd, 58, from Upton in Cheshire, was a grandfather-of-16, had served in the Royal Irish Rangers and ran a cleaning business.
He went to the hospital in July 2021 with deteriorating shortness of breath and was diagnosed with COVID-19. Syd was referred to the specialist lung department the following month for further tests.
In September, a junior doctor told Syd that there was nothing to worry about and gave him unfounded reassurance that he would be all right when they did not know this would be the case.
On 1st November, Syd was seen by a consultant who noted in a letter to his GP that he had pulmonary fibrosis, a type of lung disease that makes it hard to breathe. The consultant did not send Syd the letter or tell him about the diagnosis as they should have.
Syd found out that he had pulmonary fibrosis, a progressive and terminal illness, when he spoke to his GP in December. Syd died in August 2022.
Syd’s daughter Chantelle, 32, said:
“We feel completely let down by the Trust. My dad thought he was going to get better, because that’s what they led him to believe. Because of that he carried on working even though it was a struggle for him.
“If he had known the truth, he would have given up work and made the most of the time he had left with his family. By the time he was given the information to make that decision he was too poorly to work anyway, he was practically bed-bound. We all lost that time to spend together.
“It was such a rollercoaster. This has affected all of us and we’ve all lost our trust in the NHS. A relative offered to pay for my dad to have treatment privately, but he had such faith in the NHS that he turned it down.
“Medical staff have a duty of care to tell patients what is really happening. It was very traumatic for us all to lose him after being told that he would be fine.”
The Ombudsman found that Syd was given false reassurances about his prognosis which prevented him from making informed decisions about his health and meant he was not prepared when later told that his illness was extremely serious.
Hospital staff failed to listen to Syd’s family. Consultations were not recorded properly in his medical records, and sometimes not recorded at all.
The Countess of Chester Hospital NHS Foundation Trust took over a year to respond to the family’s complaint. The Trust did not adequately investigate what happened or acknowledge all its failings. This meant Syd’s family had to go through an unnecessarily long and painful process to get the answers they were seeking.
The Trust also failed to properly acknowledge the impact its failings had on Syd and his family and, most importantly, to learn from what had happened. While the Trust acknowledged that it had provided false reassurance to Syd, it had not taken adequate steps to make sure this does not happen again.
PHSO found no failings with the clinical care given to Syd.
Rebecca Hilsenrath added:
“We found some poor record keeping which can affect a Trust’s ability to understand the impact of what happened and to take appropriate steps to prevent it from reoccurring.
“Poor quality investigations and unacceptable delays in responding to complainants are issues we have highlighted before in the NHS. We routinely see Trusts fail to accept errors or acknowledge the impact, which causes complainants more distress at what is already a difficult time.”
PHSO recommended the Trust acknowledge its failings and apologise to Syd’s family, make service improvements, improve its record keeping, and pay Syd’s wife £1,200. The Trust has complied.
Pictured - William Chapman, known as Syd.
 Patients benefiting from gold standard safety at the Countess of Chester Hospital
Patients benefiting from gold standard safety at the Countess of Chester Hospital
 Chester Glows Green for Clatterbridge Cancer Charity
Chester Glows Green for Clatterbridge Cancer Charity
 An open letter to Chester FC supporters from Calum McIntyre
An open letter to Chester FC supporters from Calum McIntyre
 Chester FC - Club Statement
Chester FC - Club Statement
 Blues Match Report: Chester 2 - 1 Spennymoor Town
Blues Match Report: Chester 2 - 1 Spennymoor Town
 Blues Match Preview: Chester FC v Spennymoor Town
Blues Match Preview: Chester FC v Spennymoor Town
 Council approves budget to continue investing in communities
Council approves budget to continue investing in communities
 Cannabis farm sniffed out in Ellesmere Port
Cannabis farm sniffed out in Ellesmere Port
 Hundreds to turn Chester’s streets green to raise money for Clatterbridge Cancer Charity
Hundreds to turn Chester’s streets green to raise money for Clatterbridge Cancer Charity
 Major step forward as powers move from Westminster to Cheshire and Warrington
Major step forward as powers move from Westminster to Cheshire and Warrington
 Police warn Nissan Navara owners to be vigilant following thefts
Police warn Nissan Navara owners to be vigilant following thefts
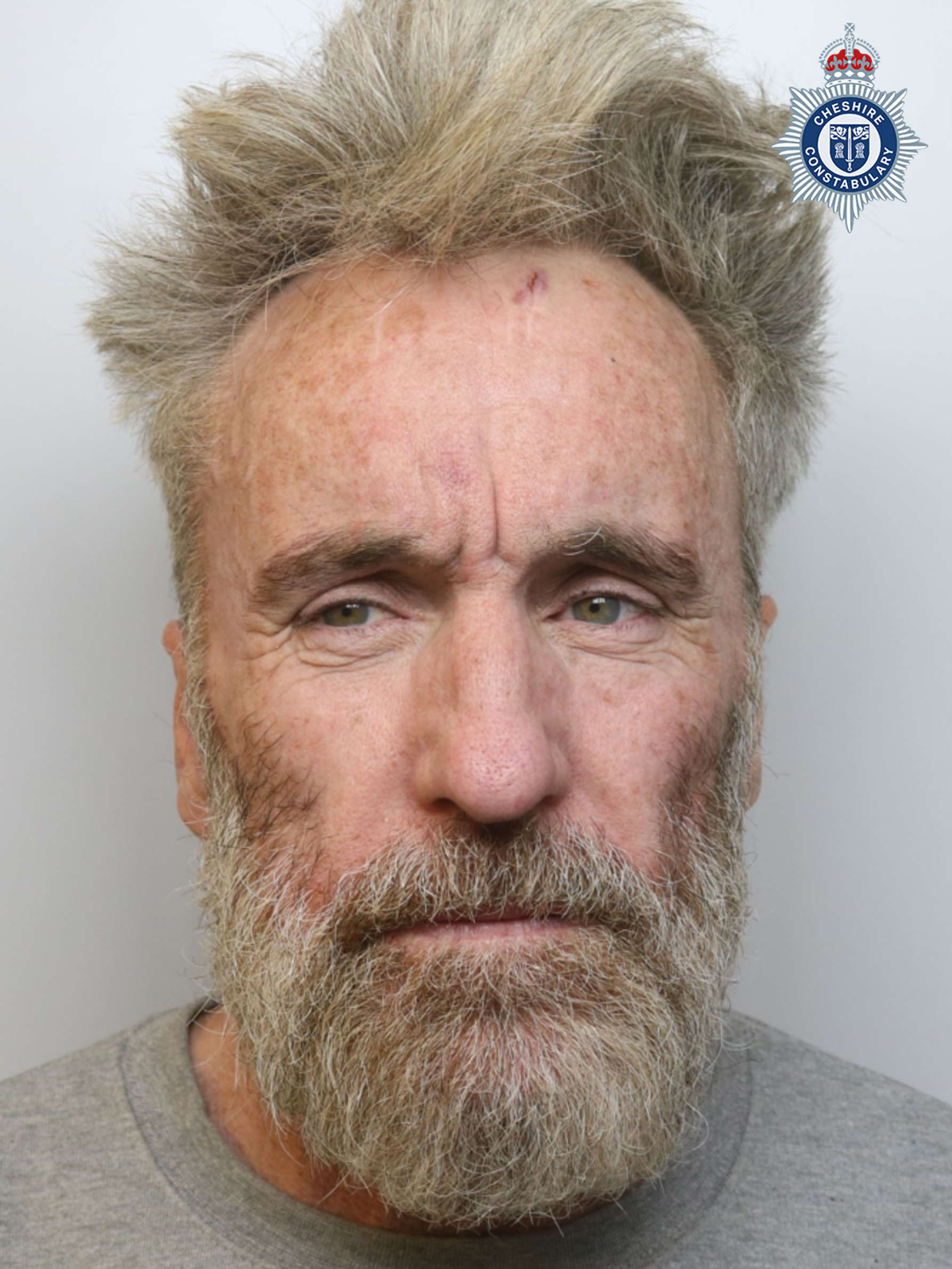 Chester man found guilty of murder
Chester man found guilty of murder
 Blues Match Report: Hereford 5 - 2 Chester
Blues Match Report: Hereford 5 - 2 Chester
 Public toilets could be spared closure under Community Asset Transfer plans
Public toilets could be spared closure under Community Asset Transfer plans
 Cheshire Police Commissioner called on to apologise for misleading public over cost of Land Rover
Cheshire Police Commissioner called on to apologise for misleading public over cost of Land Rover
 Man charged with 39 offences related to online grooming
Man charged with 39 offences related to online grooming
 Chester and Wirral Football League - Weekend Round Up
Chester and Wirral Football League - Weekend Round Up
Comments
Add a comment